The social burden of HAE
Besides the physical and psychological burden of HAE that patients experience, the disease can impact patients’ social activities and relationships. Patients can experience guilt about passing HAE onto their children, which might impact their decision on whether to have their own children.1 HAE attacks can also affect patients’ social wellbeing, as their ability to attend social/family events, participate in sports and travel may be hindered.10
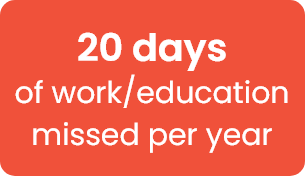
It is important to discuss with your patients about how HAE may affect their work, education and social lives, and on the importance of treatment and disease management plans to help prevent their attacks and allow them to live a more normal life.